
Introduction
In 2017, Munich Re Life US published a white paper entitled “Drug abuse mortality in the insured population.” Back then, we were seeing a rise in substance abuse deaths in the general population fueled by opioid abuse. Using a college-educated subset of the general population as a proxy for an insured population, we determined that substance abuse mortality in the general population was significantly higher than the insured experience. These were reassuring results. However, we resolved to continue to watch the trends closely.
On the positive side, efforts to increase awareness about the overdose risk of opioids, including guidelines from the Centers for Disease Control (CDC) on the effectiveness and safety of pain treatment, spurred a fall in opioid prescription rates beginning in 2017.1 However, death rates continued to climb, fueled by a dramatic rise in synthetic opioid deaths, which began ticking up in 2014 (Figure 1).
Then the pandemic hit. Drug and alcohol consumption patterns changed. Home alcohol sales increased as people attempted to cope with the COVID-19 restrictions, and deaths involving alcohol likewise increased during the pandemic.2 Opioid deaths also continued to increase sharply during the pandemic years (Figure 1). Did the pattern also change for drug abuse mortality in the insured population? Using updated population data, Munich Re set out to answer this question using methodology similar to that used before.
Substance abuse mortality in the general population
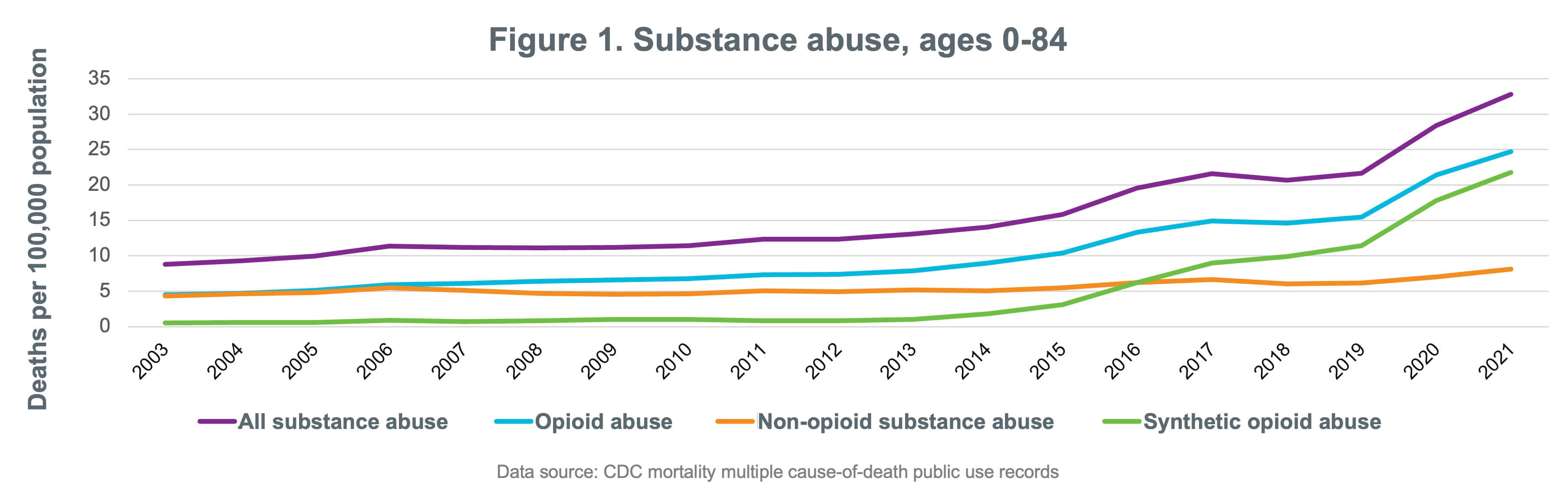


We continue to focus our analysis at the substance abuse level, not specifically drilling down to opioids. Due to the way the cause of death is recorded in the databases, drilling down any further could lead to a higher level of misclassification risk. However, Figure 1 shows that almost all of the increase in drug-related mortality over the period being considered comes from opioids (including synthetic opioids), so conclusions drawn at this level should reasonably translate to the subset of opioid abuse.
We used two main data sources in this analysis: the Mortality Multiple Cause-of-Death Public Use Records from the CDC and Munich Re’s proprietary cause-of-death experience study. The CDC data were based on the general U.S. population and included more than 920,000 deaths from substance abuse between 2003 and 2021. Munich Re’s study was based on life insurance claims data and comprised more than 2,000 substance abuse deaths from 2006 to 2021.
A socio-economic view of the crisis
Using the same methodology as before, we began our investigation by splitting the population experience by socio-economic level. Since the CDC data did not include any measure of income or wealth, we used the highest educational level attained as a proxy. We split the mortality rate per 100,000 into four main categories of educational attainment (no degree, high school degree, some college, and college degree). Most of the rise in substance abuse mortality in the general population can be explained by the dramatic 115% increase in mortality in the recent five-year period 2016-2021 for the lower academic attainment experience (Figure 2).
We continue to see that the mortality rate due to substance abuse is significantly lower with higher academic attainment. We have not attempted to explain the correlation between higher education and lower substance abuse-related deaths, however, our previous paper supported our hypothesis that the college-educated sub-group was a good proxy for the insured population.3 While the subsets of the population with the highest academic attainment had the flattest mortality trend over time, it is important to recognize that this group still experienced a 25% increase in substance abuse death rate over the recent five-year period of 2016-2021 (Figure 2).

Substance abuse mortality in the insured population
We compared the mortality rates for the college-educated population with updated life insurance claims experience from our own block of reinsurance business split into two segments: first, claims that occurred in policy durations one to 15 (to approximate the select period) and second, claims that occurred in policy durations 16 and later (to approximate an ultimate period). When we looked at the mortality rate by attained age (Figure 3), we saw that the mortality rate for the college-educated population continued to be a reasonable proxy for the insured mortality rate in the ultimate period, particularly at younger ages. We also observed that the select rate was significantly lower than the ultimate rate, implying that good protective value continues to be derived from the underwriting process.
When we compare the updated cause-of-death rankings between the general population (Table 1) and the college-educated population (Table 3), a surprising result emerges for the college-educated population (Table 3). Substance abuse is now the leading cause of death for both the general and college-educated populations for ages 30-39. This is a jump from the previous #5 cause of death in this age group among the college-educated population. In all other age groups, the general public continues to rank higher than the college-educated sub-population for substance abuse deaths. However, for the college-educated ages 40-49, we also see a jump to #3 cause of death versus not even in the top 5 for the college-educated 40-49 age group in 2017. For college-educated ages 20-29 and 50-59, there has been no change (Table 4).



Risk selection considerations
This analysis provides evidence that there may be a way to approximate the impact on life insurance mortality using the readily available college-educated subset of the population data. However, some key filters will be missing in the population databases, e.g., issue age and duration. In this section, we will provide some insights into these views using Munich Re’s proprietary cause-of-death experience study.
Duration
We analyzed the substance abuse mortality rate by policy duration to see if the select period showed any evidence of early-duration adverse selection. Adjusting for age, we would expect that the mortality rate would start off lowest in duration one and gradually increase in an exponential curve. The data show this pattern with a noticeable selection effect and no evidence of adverse selection. We also looked at the percentage of claims that are due to substance abuse, which shows a slightly decreasing trend. This is as expected since as underwriting wears off, medical causes of death such as circulatory system and neoplasm represent a larger percentage of total claims, pushing down the share of substance abuse claims.
Issue Age
We analyzed the mortality rate and the percentage of claims that are due to substance abuse by issue age to see if there were any unexpected spikes in the pattern. For issue ages 20-29, the data show evidence of adverse selection since there was a jump in both the mortality rate and the ratio of substance abuse deaths to total deaths. Otherwise, the pattern is as expected.
Conclusion
Opioid deaths have continued to increase sharply in the general population, fueled by a dramatic rise in synthetic opioid deaths, which began ticking up in 2014, and continued increasing during the pandemic years. Sadly, substance abuse deaths also increased in all age groups in the general population under 60 years old with substance abuse now the #1 cause of death for those in their 20s and 30s. Most of the rise in substance abuse mortality can be explained by the dramatic 115% increase in mortality in the recent five-year period 2016-2021 for the lower academic attainment experience.
More notable from a life insurance perspective is the 25% increase in substance abuse death rate among the college-educated group (our insured population proxy) over the recent five-year period 2016-2021. In fact, mortality in all ages of the college-educated group is increasing, with a particular concern for ages 30-39, as substance abuse is now the leading cause of death for both the general and college-educated populations. Since synthetic opioids are the main causative factor in the general population, it is not unreasonable to assume that synthetic opioids are also the main culprit of the rise in substance abuse deaths in the college-educated group.
While substance abuse deaths are increasing much higher in those with lower academic attainment, the rise in college-educated substance abuse deaths (especially those ages 30-39) is a particularly concerning trend for the insurance industry and must be followed closely. Underwriting departments should analyze the protective value of current underwriting requirements in order to guard against anti-selection. Munich Re’s internal research provides evidence that substance abuse misrepresentation can be effectively captured by digital medical data, such as electronic health records (EHRs). Other possible mitigating solutions include opioid marker urine or blood screens, added questionnaires, prescription data, and/or medical claims data.
It is important to remember, however, that prescription data will not catch illicit, synthetic, non-prescription drugs. Medical claims data will help only if there is a diagnosis of abuse or addiction. Opioid screening protocols involve blood and/or urine testing that are generally not included in clinical labs, so adding insurance labs may not be the best choice, especially for automated underwriting programs. On a positive note, our data shows that current underwriting processes are still providing significant selection benefits for our target market for life insurance. We continue to partner with our clients to better understand and mitigate these risks.
References
Contact
/Gina%20Guzman.jpg/_jcr_content/renditions/original./Gina%20Guzman.jpg)

Related Solutions
properties.trackTitle
properties.trackSubtitle



