
Living with, Rather than Dying from, HIV:
Insurance Updates and Insights into HIV Infection
properties.trackTitle
properties.trackSubtitle
Introduction
The course of HIV infection was markedly altered by the introduction of combination antiretroviral therapy in 1996. Despite the absence of a cure, persons with HIV infection who are without significant comorbidities and are treated before significant immunosuppression occurs have a life expectancy approaching that of the general population. Advances in treatment, the initiation of treatment at earlier stages, and improvements in compliance have dramatically improved both mortality and morbidity.
We find standardized mortality ratios for persons living with HIV (PLWH) who are adherent to treatment, responding well to treatment, and have no significant comorbidities to be within insurable ranges for most age groups. Moreover, we have found rates of potentially disabling conditions to be only modestly increased in those with well-controlled HIV infection and no significant comorbidities. Besides qualifying for life coverage, some of those living with HIV also now qualify for disability coverage.
Background
Human Immunodeficiency Virus (HIV) is a retrovirus that infects and destroys CD4+ T lymphocytes, one of the body’s important immune defenses. It is spread through exposure to body fluids, most often through sexual activity, shared needles, or childbirth. HIV can usually be readily diagnosed with a simple blood test.
Once an individual is infected with HIV, replication begins, but the rate of progression depends on a complex interplay of immune functions. Given the ability of HIV to quickly incorporate its genetic material into the DNA of the T lymphocyte, eradication of the infection is not currently feasible. Left untreated, most will progress to acquired immune deficiency syndrome (AIDS), though approximately 7% of those with HIV remain asymptomatic and about 1 in 300 become non-viremic "elite controllers” with a favorable course despite no treatment.
In most cases, once positive HIV test results are confirmed, viral levels and CD4 cell counts are obtained and treatment with combination anti-retrovirus therapy (ART) is initiated. ART has become very effective at keeping the virus level suppressed and decreasing the risk of transmission – in many cases converting acute HIV infection into a chronic, manageable disease. This is possible as long as effective treatment is maintained in combination with good medical follow-up.
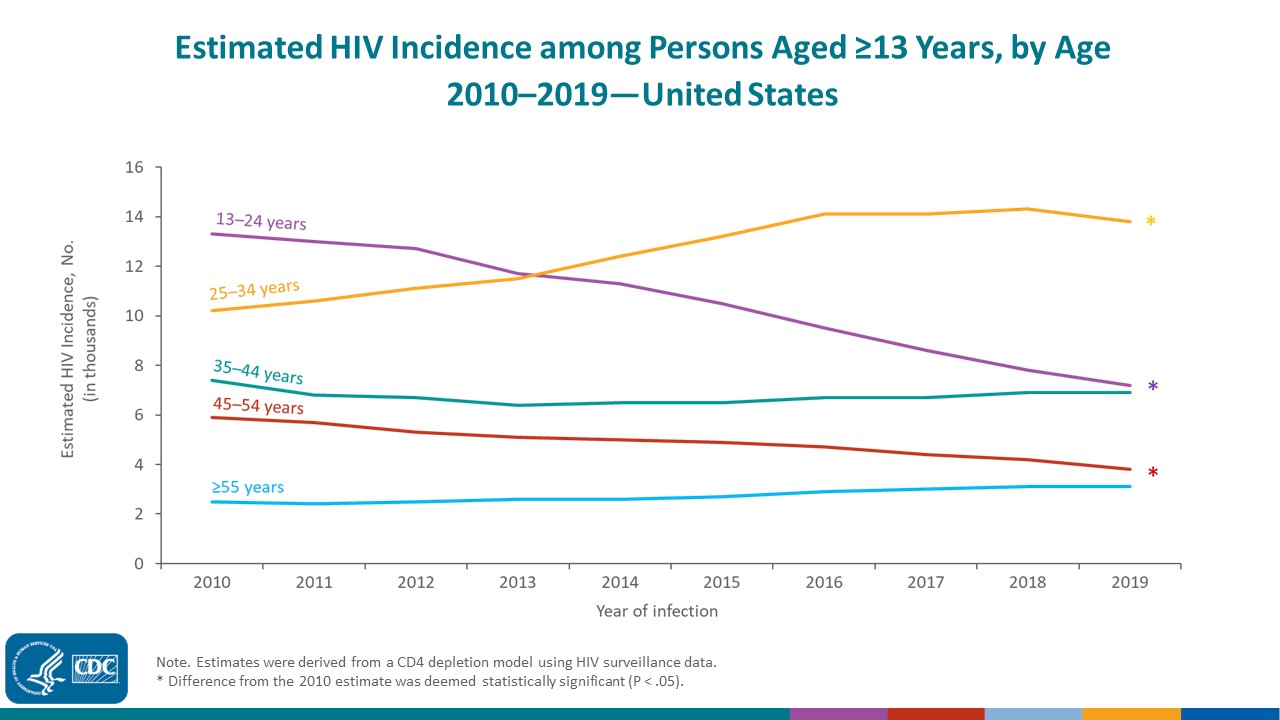
HIV Incidence
HIV Prevalence
Mortality Trends over Time
Since the introduction of ART in 1996, the life expectancy for PLWH has increased markedly. Medical advancements have changed treatment regimens from multiple pills taken multiple times per day to often a single pill per day. This helps further improve outcomes by dramatically increasing treatment compliance.
Studies based on more recent datasets have consistently shown an improvement in mortality. These are, of course, limited by shorter duration of follow-up. But this finding is consistent with an overall decline in AIDS diagnoses, improved ART regimens, and the current practice of initiating ART at diagnosis rather than when CD4 counts reached <500, as was usual in the past.
Those with HIV infection do have higher rates of significant comorbidities (such as smoking, drug and alcohol use, and cardiovascular and psychiatric risks) than those without HIV infection, making mortality comparisons more difficult. When adjusting for these factors as much as is feasible, it is evident that mortality rates for those without these comorbidities are much lower, though still higher than for a similar group without HIV infection.
Morbidity Trends over Time
Even with the availability of effective treatment, complications from chronic HIV infection – or from the treatment itself – can occur. This contributes to higher rates of morbidity and resultant limitations for PLWH as a group.
Studies have found that PLWH have decreased quality-adjusted years of life and develop evidence of comorbidities (e.g., cardiovascular disease, osteoporosis, cognitive dysfunction, and certain malignancies) more frequently and at younger ages compared with individuals without HIV. Much of this added risk appears to be related to a higher prevalence of comorbid conditions and behaviors, though additional risk is also thought to be due to long-term ART use and sustained HIV-induced immune activation and inflammation. It is believed that chronic inflammation can lead to accelerated aging and an increased risk of developing multiple comorbidities as PLWH age.
Although the risk for multimorbidity is higher among PLWH throughout the age cycle, this risk appears to be relatively low in those with well-controlled HIV infection and without important comorbid risks.
Conclusion
Today’s HIV-positive population is considerably different than it was in the past. Better treatments that begin earlier after infection and are easier to comply with have dramatically improved both mortality and morbidity for PLWH. As long as effective treatment is maintained, in combination with good medical follow-up, acute HIV infection is often converted into a chronic, manageable disease.
Our analysis concludes that mortality rates for this population, although remaining higher than expected, are now definitely priceable for an insurance portfolio. In addition, we find that those with well-controlled HIV infection and no significant comorbidities can now also qualify for disability coverage.
For more information regarding Munich Re Life US’s medical research supporting mortality and morbidity improvements for PLWH, contact Dr. Gina Guzman and Dr. Brad Heltemes.
/Gina%20Guzman.jpg/_jcr_content/renditions/original./Gina%20Guzman.jpg)
/Brad%20Heltemes.jpg/_jcr_content/renditions/original./Brad%20Heltemes.jpg)