Prediabetes and hemoglobin A1c levels in non-diabetics
2017/11/15
properties.trackTitle
properties.trackSubtitle

What underwriters should know
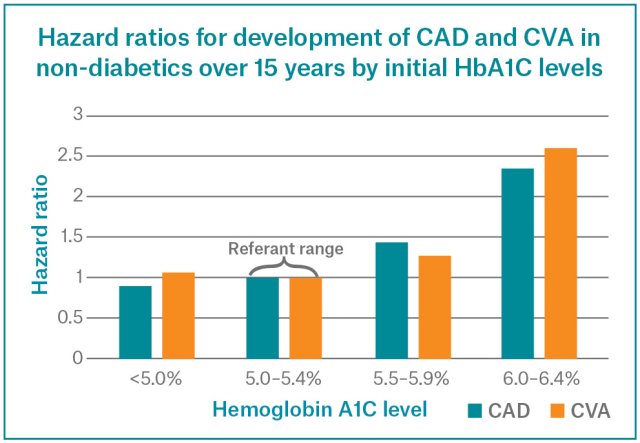
- Hemoglobin A1C (HbA1C) levels above 5.4 percent in nondiabetics are associated with increased relative risk for developing coronary atherosclerotic heart disease (CAD), ischemic stroke (CVA) and mortality from any cause, as compared to those with HbA1C levels in the 5.0–5.4 percent range.
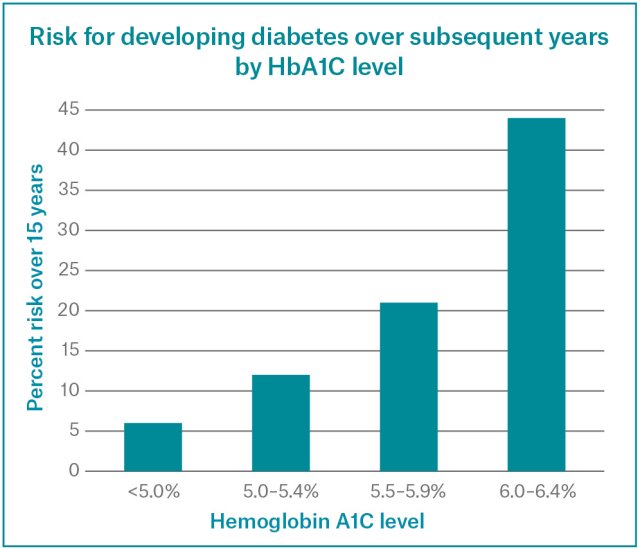
- Risk of developing diabetes mellitus over the ensuing fifteen years approximately doubles for each band of HbA1C from 5.0–5.4 percent, 5.5–5.9 percent and 6.0–6.4 percent.
- Underwriters observing HbA1C levels below 6.5 percent in nondiabetic individuals should not assume there is no associated increase of risk. As with any prudent underwriting assessment, it is essential to consider all risk factors presented before determining a final decision.
Today, prediabetes is a new word for a fast-rising problem around the world: an often undiagnosed metabolic condition which could lead to a more serious diagnosis of diabetes mellitus down the line. As many as 5.7 million Canadians can be considered to have prediabetes.1 The trouble is, many do not know they have it, and prediabetes often has no symptoms at all. Yet if steps aren’t taken to control their blood sugar now, nearly 50 percent will go on to develop type 2 diabetes.1
What is prediabetes? Is it important?
Prediabetes, also known as ‘impaired fasting glycemia’ (IFG) and ‘impaired glucose tolerance’ (IGT) is a metabolic condition with no symptoms. An additional prediabetes state also exists that arises transiently during pregnancy, otherwise known as gestational diabetes.
Prediabetes is a growing global problem that is closely linked to obesity and is almost always a precursor to the development of type 2 diabetes. It is characterised by the presence of higher than normal blood glucose levels that are yet to reach diabetic levels. Physicians now understand that the health complications associated with type 2 diabetes often occur before a medical diagnosis is made.
With HbA1c testing, can a diagnosis of diabetes mellitus be considered?
What are the risks associated with prediabetic HbA1c levels below 6.5 percent?
Are there also risks associated with HbA1C levels below 5 percent?
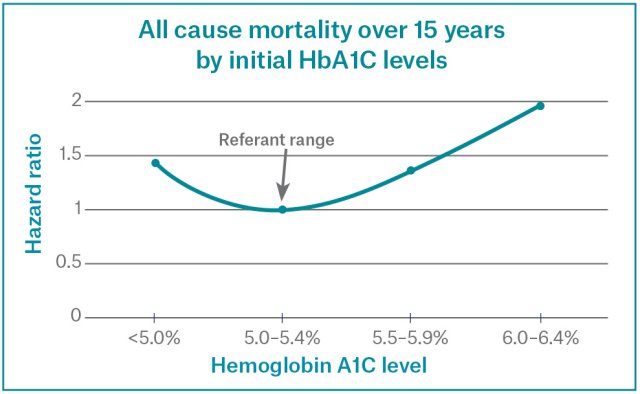
With such processes associated with rapid red blood cell turnover, splenomegaly, or the necessity for blood transfusion may well be indicative of underlying conditions associated with increased mortality. However, the J-shaped mortality curve remains after significant hematologic problems are excluded, suggesting that further evaluation of health problems associated with the low-normal glycemic state need to be investigated.
In addition to macrovascular disease, are there other risks associated with low HbA1c levels?
Specific diseases associated with the increased mortality found in low HbA1C levels have not been well defined, but there appears to be an increase in cancer-related deaths.4 Interestingly, an association between low HbA1C values and hospitalization for liver disease has also been found.
Conversely, hematologic problems may also result in falsely elevated HbA1C levels. For example, when red blood cell production is depressed in some anemic states (e.g., untreated iron deficiency, vitamin B 12 deficiency or folate deficiency), a disproportionate number of older red blood cells may result in a false elevation of HbA1C levels. Values may also be falsely high in the presence of abnormal hemoglobin e.g. Fetal hemoglobin (HbF) or isckle hemoglobin (HbS). Whereas chronic kidney disease may result in either falsely depressed or falsely elevated values.
Underwriting and the future
With the increasing number of new cases of prediabetes on a global scale, and recognising the causal relationship between this condition and vascular disease, Munich Re’s view is that underwriters need to be aware more than ever of the implications this condition can have on mortality and morbidity. As with any prudent underwriting assessment, it is important to consider all risk factors presented before determining a final decision.
1. Canadian diabetes association
2. Selvin E, et al, Glycated Hemoglobin, Diabetes, and Cardiovascular Risk in Nondiabetic Adults, NEJM 2010,362(9):800–11.
3. Stout R, et al, Relationship of Hemoglobin A1c to Mortality in Nonsmoking Insurance Applicants, Journal of Insurance Medicine 2007;39:174–81.
4. Aggarwal V, et al, Low Hemoglobin A1c in Nondiabetic Adults, Diabetes Care 2012,35:2055–2060.
/Tim%20Meagher%202019.jpg/_jcr_content/renditions/original.image_file.120.120.file/Tim%20Meagher%202019.jpg)
.jpg/_jcr_content/renditions/original.image_file.120.120.file/Reece%20Hodgson%202014%20(preferred).jpg)